Are you looking to understand how high-flow nasal cannula oxygen therapy is revolutionizing respiratory support? This article dives deep into the benefits, applications, and advantages of this advanced oxygen delivery method. We’ll explore why it’s becoming a game-changer in healthcare, offering a more comfortable and effective way to deliver supplemental oxygen. Keep reading to discover how high-flow nasal cannula therapy can improve patient outcomes and streamline respiratory care.
1. What is High-Flow Nasal Cannula Oxygen Therapy and Why is it a Superior Oxygen Delivery System?
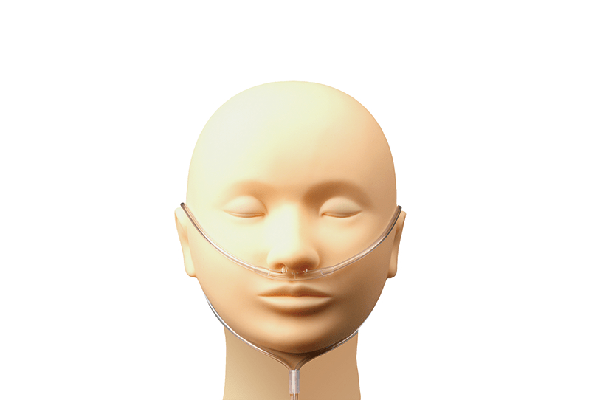
High-flow nasal cannula (HFNC) oxygen therapy is an advanced method of providing respiratory support to patients who need supplemental oxygen. Unlike traditional oxygen delivery systems, HFNC can deliver oxygen at significantly higher flow rates, often ranging from 3 to 50 times the flow of a standard nasal cannula. This capability to deliver high flow oxygen is what sets it apart and makes it a superior oxygen delivery system in many clinical situations.
Traditional methods, such as simple nasal cannulas or face masks, are considered low-flow oxygen therapy. These systems typically deliver oxygen at flow rates up to 6 liters per minute (LPM). In contrast, high-flow nasal cannula therapy can deliver flow rates up to 60 liters per minute, and sometimes even higher. This higher flow rate provides several advantages. Firstly, it can more effectively meet a patient’s inspiratory demands, especially in cases of increased respiratory rate or distress. Secondly, the heated and humidified oxygen delivered via nasal high flow helps to improve patient comfort and reduce drying of the nasal mucosa, a common issue with traditional oxygen therapy. Because of its ability to deliver a more precise and comfortable oxygen therapy delivery, HFNC is increasingly favored in various healthcare settings.

2. How Does High-Flow Nasal Cannula Therapy Differ from Traditional Low-Flow Oxygen Therapy?
The fundamental difference between high-flow nasal cannula therapy and low-flow oxygen therapy lies in the flow rate of oxygen delivered to the patient. Low-flow systems, like standard nasal cannulas, are designed to deliver oxygen at flow rates of up to 6 LPM. These are suitable for patients who need a relatively small amount of supplemental oxygen. However, the concentration of oxygen actually delivered by low-flow systems can be variable and depends on the patient’s respiratory rate and tidal volume. A simple nasal cannula can only effectively provide a limited fraction of inspired oxygen (FiO2), and this is often not precisely controlled.
High-flow nasal cannula therapy, on the other hand, utilizes a specialized device to deliver heated and humidified oxygen at flow rates ranging from 15 up to 60 LPM, and sometimes even higher. This significantly higher flow provides a more consistent and predictable oxygen concentration to the patient. Furthermore, the heated and humidified aspect of high-flow nasal cannula oxygen therapy is crucial. Traditional low-flow oxygen, especially when delivered at higher concentrations, can be dry and irritating to the nasal passages and airways. Heated and humidified oxygen helps to prevent drying of the nasal mucosa, reduces airway resistance, and improves mucociliary clearance – the natural process of clearing mucus from the airways. This makes high-flow nasal cannula therapy a more comfortable and physiologically beneficial type of oxygen therapy, especially for patients requiring prolonged or high levels of oxygen support.
3. What are the Key Benefits of High-Flow Nasal Cannula Therapy for Patients in Need of Oxygen Therapy?
High-flow nasal cannula therapy offers a multitude of benefits for patients who need oxygen therapy. One of the primary advantages is improved oxygenation. By delivering oxygen at high flow rates, HFNC can meet or exceed the patient’s inspiratory flow demands, ensuring a more stable and higher fraction of inspired oxygen. This is particularly beneficial for patients with respiratory distress or those who are working hard to breathe. For example, a patient with pneumonia or acute respiratory distress syndrome (ARDS) may have a very high respiratory rate and require a significant amount of oxygen. High-flow nasal cannula therapy can effectively deliver the necessary supplemental oxygen in these situations.
Another significant benefit is enhanced patient comfort. The heated and humidified oxygen is much gentler on the nasal passages compared to dry, cold oxygen from traditional systems. This reduces nasal dryness, irritation, and discomfort, improving patient tolerance and compliance with oxygen therapy. Patients are also able to eat, speak, and cough more easily with a nasal cannula compared to a tight-fitting face mask, further enhancing their comfort.
Furthermore, high-flow nasal cannula therapy can reduce the work of breathing. The high flow of gas can create a small amount of positive airway pressure, which helps to keep the small airways in the lungs open and reduces the effort required to breathe. This is particularly helpful for patients with conditions like chronic obstructive pulmonary disease (COPD) or heart failure, where breathing can be labored. Clinical studies have also shown that high-flow nasal cannula therapy can reduce the need for intubation and mechanical ventilation in some patient populations, leading to better outcomes and shorter hospital stays. Overall, the combination of improved oxygen delivery, enhanced comfort, and reduced work of breathing makes high-flow nasal cannula therapy a powerful tool in respiratory care.
4. In What Medical Scenarios is High-Flow Nasal Cannula Therapy the Preferred Oxygen Delivery Method?
High-flow nasal cannula therapy has become a preferred oxygen delivery method in a wide range of medical scenarios, particularly in situations where patients require significant respiratory support but are not yet in need of or ready for mechanical ventilation. One common application is in the treatment of acute respiratory failure. Patients with conditions such as pneumonia, bronchiolitis (especially in children), and acute exacerbations of COPD often benefit from high-flow nasal cannula therapy. In these cases, it can help to improve oxygenation, reduce respiratory distress, and potentially avoid the need for more invasive interventions like intubation.
Post-extubation support is another key area where high-flow nasal cannula is increasingly utilized. After a patient has been on mechanical ventilation and is extubated (breathing tube removed), they are at risk of respiratory distress or failure. Several studies, including research on the effect of postextubation high-flow nasal cannula, have demonstrated that using a high-flow nasal cannula post-extubation can reduce the risk of reintubation compared to traditional low-flow oxygen or simple nasal oxygen. This is particularly important in patients who are considered high-risk for respiratory complications after extubation.
In the emergency department, high-flow nasal cannula can be valuable for rapid oxygenation in patients presenting with severe respiratory distress. It allows for quick and effective supplemental oxygen intervention without the need for tight-fitting masks, which can be poorly tolerated. Moreover, in palliative care settings, high-flow nasal cannula can provide comfortable and effective oxygen therapy for patients with end-stage respiratory illnesses, improving their quality of life by alleviating breathlessness. The versatility and efficacy of high-flow nasal cannula make it a valuable tool across various medical specialties and patient populations needing significant respiratory support.

5. How Does High-Flow Nasal Cannula Improve Patient Comfort and Tolerance Compared to Other Oxygen Delivery Devices?
Patient comfort and tolerance are significantly improved with high-flow nasal cannula therapy compared to many other oxygen delivery devices, especially traditional face masks. One of the primary reasons for this enhanced comfort is the humidification and heating of the oxygen. Traditional oxygen therapy, particularly at higher flow rates, delivers dry, unconditioned gas directly into the nasal passages. This can lead to significant drying of the nasal mucosa, causing discomfort, nosebleeds, and increased mucus production. The heated oxygen in high-flow nasal cannula therapy counteracts this drying effect, maintaining mucosal hydration and comfort.
Face masks, while capable of delivering high concentrations of oxygen, often feel claustrophobic and restrictive to patients. They can also make it difficult to eat, drink, or communicate effectively. In contrast, a nasal cannula, even a wide-bore nasal prong used for high flow, is less intrusive. Patients can more easily eat, speak, and cough without interrupting their oxygen therapy when using a high-flow nasal cannula. This is particularly beneficial for patients who require long-term oxygen support or those who are alert and communicative.
Furthermore, the nasal cannula allows for better clearance of secretions. With face masks, secretions can pool underneath the mask, potentially increasing the risk of aspiration or discomfort. The open nature of the nasal cannula allows for easier expectoration of secretions, promoting airway hygiene. The combination of humidified and heated oxygen, less restrictive interface, and improved ability to eat and communicate makes high-flow nasal cannula a much more patient-friendly option compared to many traditional oxygen delivery devices. This improved comfort can lead to better patient compliance, longer duration of therapy when needed, and overall a more positive experience with oxygen therapy.
6. What Flow Rate is Typically Used in High-Flow Nasal Cannula Oxygen Therapy and How is it Adjusted?
The flow rate used in high-flow nasal cannula oxygen therapy is highly variable and depends on the individual patient’s needs and clinical condition. Unlike low-flow nasal cannula, where flow rates are typically capped at 6 LPM, high-flow systems can deliver flow rates up to 60 LPM, and in some cases even higher. The initial flow rate is usually set based on the patient’s respiratory distress and oxygen saturation levels. A common starting point might be around 20-30 LPM, but this is just a general guideline and must be individualized.
The flow rate is carefully titrated, or adjusted, based on continuous monitoring of the patient’s clinical response. Key parameters monitored include oxygen saturation (SpO2), respiratory rate, heart rate, and work of breathing. The goal is to achieve and maintain adequate oxygen saturation (typically above 92-94%, but targets may vary depending on the patient’s condition) while minimizing signs of respiratory distress. If the patient’s oxygen saturation is low or they are still showing signs of increased respiratory effort, the flow rate may be gradually increased. Conversely, if the oxygen saturation is consistently high and the patient is comfortable, the flow rate might be reduced to the lowest effective level.
The adjustment of flow rate is a dynamic process that requires close observation and clinical judgment. It’s not just about achieving a target oxygen saturation number, but also about assessing the patient’s overall clinical picture. Factors like the underlying cause of respiratory distress, the patient’s age, and any comorbidities also influence flow rate adjustments. Regular assessment and titration by healthcare professionals are crucial to optimize high-flow nasal cannula therapy and ensure it meets the patient’s evolving respiratory needs.
7. Is High-Flow Nasal Cannula Effective for Emergency Oxygen Administration and Respiratory Distress?
Yes, high-flow nasal cannula is indeed effective for emergency oxygen administration and in managing patients with respiratory distress. Its rapid onset of action and ability to deliver high concentrations of oxygen quickly make it a valuable tool in emergency situations. In cases of acute hypoxemia (low blood oxygen levels) or severe respiratory distress, timely and effective oxygen delivery is critical. High-flow nasal cannula can provide this rapid support, often more efficiently than traditional low-flow systems or even standard face masks.
In emergency settings like the emergency department or intensive care unit, patients may present with various conditions causing respiratory distress, such as acute exacerbations of asthma, severe pneumonia, or acute heart failure. In these scenarios, using a high-flow nasal cannula allows for immediate supplemental oxygen therapy. The high flow rates can quickly improve oxygen saturation levels and alleviate some of the work of breathing, providing crucial support while further diagnostic and treatment measures are being implemented.
Compared to other emergency oxygen devices like non-rebreather masks, high-flow nasal cannula offers several advantages in the acute setting. It is generally better tolerated, allowing for longer periods of application without significant discomfort. It also allows for easier communication and access for oral intake, which is important in a dynamic emergency situation. Furthermore, the heated and humidified oxygen can be beneficial from the start, reducing airway irritation and improving overall respiratory mechanics. While high-flow nasal cannula may not be suitable for every emergency respiratory situation (e.g., in cases needing immediate and very high FiO2 or airway protection), it is a highly effective and increasingly preferred option for many patients experiencing acute respiratory distress requiring supplemental oxygen.
8. What are the Potential Risks and Considerations When Using High-Flow Nasal Cannula Therapy?
While high-flow nasal cannula therapy is generally safe and well-tolerated, there are potential risks and considerations that healthcare providers must be aware of. One important consideration is the potential for barotrauma, or lung injury from excessive pressure. Although high-flow nasal cannula delivers relatively low levels of positive airway pressure compared to mechanical ventilation, very high flow rates, particularly in patients with certain lung conditions, could theoretically lead to lung overdistension or injury. Therefore, careful monitoring of respiratory mechanics and appropriate flow rate titration are essential.
Another consideration is the risk of oxygen toxicity. While less common with nasal cannula oxygen versus higher FiO2 delivery methods like masks, prolonged exposure to high concentrations of oxygen can lead to pulmonary oxygen toxicity. This is more of a concern when using high-flow nasal cannula for extended periods at very high FiO2 settings. The fraction of inspired oxygen should be titrated down as soon as clinically feasible to minimize this risk.
Nasal irritation and dryness, although less pronounced than with traditional dry oxygen, can still occur in some patients, especially with prolonged use. While the humidification system is designed to mitigate this, regular assessment of nasal mucosa and appropriate adjustments to humidification levels are important. In rare cases, patients may develop nasal passage irritation or even minor nosebleeds.
Finally, it’s crucial to recognize that high-flow nasal cannula is not a substitute for mechanical ventilation in all cases. In patients with severe respiratory failure who are not responding to HFNC or who have contraindications to its use, timely escalation to mechanical ventilation is necessary. Delaying intubation when it is truly needed can have adverse consequences. Therefore, careful patient selection, continuous monitoring, and a clear understanding of the indications and limitations of high-flow nasal cannula therapy are vital for its safe and effective application.
9. How Does High-Flow Nasal Cannula Impact Oxygen Saturation and Overall Respiratory Function?
High-flow nasal cannula therapy has a significant positive impact on oxygen saturation and overall respiratory function in patients who need supplemental oxygen. One of the primary mechanisms through which it improves oxygenation is by more effectively delivering supplemental oxygen to the lungs. Traditional nasal cannulas, especially at higher flow rates, can be less efficient at delivering oxygen due to dilution with room air and variations in the patient’s breathing pattern. High-flow nasal cannula, with its ability to provide flow rates up to 60 LPM, can better meet the patient’s inspiratory flow demands and reduce the amount of room air entrainment, thus delivering a more consistent and higher fraction of inspired oxygen, which directly translates to improved oxygen saturation.
Beyond oxygenation, high-flow nasal cannula can also improve other aspects of respiratory function. The heated and humidified gas can reduce airway resistance and improve mucociliary clearance. By reducing airway resistance, it becomes easier for patients to breathe, decreasing the work of breathing. Improved mucociliary clearance helps to clear secretions from the airways, which is particularly beneficial in patients with respiratory infections or conditions associated with mucus buildup.
Furthermore, the flow of oxygen delivered via nasal prongs can create a mild positive pressure in the airways. This positive pressure, although small, can help to keep alveoli (tiny air sacs in the lungs) open, improving gas exchange and reducing atelectasis (lung collapse). This effect is similar to, but less pronounced than, continuous positive airway pressure (CPAP) or mechanical ventilation.
Clinical studies have consistently shown that high-flow nasal cannula therapy can improve oxygen saturation, reduce respiratory rate, and decrease the work of breathing in patients with various respiratory conditions. These improvements in respiratory function contribute to better patient outcomes, reduced need for escalation to more invasive respiratory support, and enhanced overall respiratory well-being.
10. What is the Future of High-Flow Nasal Cannula in Oxygen Therapy and Respiratory Care?
The future of high-flow nasal cannula in oxygen therapy and respiratory care is very promising, with ongoing research and technological advancements expanding its applications and improving its efficacy. One key area of future development is in refining the technology and devices themselves. Manufacturers are continuously working on making HFNC systems more user-friendly, portable, and cost-effective. Advancements in humidification and heating technology could further enhance patient comfort and reduce potential complications.
Research is also ongoing to explore new clinical applications for high-flow nasal cannula. While its use in acute respiratory failure and post-extubation support is well-established, studies are investigating its potential in other areas such as pre-oxygenation before intubation, management of obstructive sleep apnea, and even in certain cardiac conditions. The efficacy of high-flow nasal cannula in various patient populations and clinical settings is being actively explored.
Another exciting direction is the integration of high-flow nasal cannula with other respiratory support modalities. Combining HFNC with non-invasive ventilation (NIV) or using it in conjunction with specific pharmacological treatments may further optimize respiratory outcomes in certain patient groups. Personalized approaches to high-flow nasal cannula therapy, tailoring flow rates and FiO2 based on individual patient characteristics and real-time physiological monitoring, are also likely to become more prevalent.
As our understanding of respiratory physiology and the mechanisms of action of high-flow nasal cannula deepens, and as technology continues to advance, HFNC is poised to play an even more central role in oxygen therapy and respiratory care in the years to come. Its versatility, efficacy, and patient-friendly nature make it a cornerstone of modern respiratory management, and future innovations will likely solidify its position as a leading oxygen delivery system.
Key Takeaways:
- High-flow nasal cannula (HFNC) therapy delivers heated and humidified oxygen at flow rates significantly higher than traditional nasal cannulas, typically 3-50 times greater.
- HFNC offers superior oxygen delivery by meeting inspiratory demands, providing a more consistent fraction of inspired oxygen, and improving oxygen saturation.
- Patient comfort is significantly enhanced with HFNC due to heated and humidified oxygen, reducing nasal dryness and irritation compared to low-flow oxygen therapy.
- HFNC is effective in various medical scenarios, including acute respiratory failure, post-extubation support, and emergency oxygen administration.
- Flow rate in HFNC is individualized and titrated based on continuous monitoring of oxygen saturation, respiratory rate, and work of breathing.
- Potential risks of HFNC are low but include barotrauma and oxygen toxicity, necessitating careful monitoring and appropriate flow rate adjustment.
- HFNC positively impacts respiratory function by improving oxygenation, reducing work of breathing, and enhancing mucociliary clearance.
- The future of HFNC is bright, with ongoing research and technological advancements expanding its applications and improving its efficacy in respiratory care.
This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment.
Internal Links:
For more information on related medical consumables, explore our range of high-quality Medical Gauze Bandage Roll and Medical Surgical Face Masks. We also offer a variety of Disposable Medical Bed Sheets suitable for hospitals and clinics. Consider our Sterile suture with needle for your surgical supply needs. For respiratory care, our Disposable PVC nasal oxygen cannula tube provides reliable oxygen delivery.
Post time: 2月-05-2025





